
The BBC was informed by a former midwife that she left the profession because she could not live with herself if she gave subpar treatment.
Staff shortages, according to Hannah Williams, meant that she occasionally had to “live by the skin of her teeth” to keep patients safe.
According to a BBC Verify research, there have been 7% more full-time equivalent midwife posts in England over the past ten years.
By contrast, there has been a 34% rise in the NHS staff as a whole.
There are almost 2,500 less midwives in the nation than there should be, and maternity centres are dealing with security issues.
Additionally, according to BBC data, more than one in five midwife positions remain empty in some trusts.
Staffing is the “most important issue” according to the Royal College of Midwives, and the deficit needs to be closed.

Every day, miracles can happen in maternity facilities.
Meeting a worried Nicole D’Cruze on the labour ward at Croydon University Hospital, we observed one.
She gave us permission to videotape the procedure because she was going to have a planned caesarean section.
The seamless collaboration between the anaesthetist, midwife, surgeon, and the remainder of the surgical team exemplified the highest standard of NHS care.
A happy and relieved tear fell down her mother’s cheek when Zenia cried out for the first time.
However, not every family has it so good.
Concerns regarding safety
There was a 67% failure rate in English units to routinely exceed safety criteria, as we revealed in our November study.
All hospital services examined by the Care Quality Commission had poor safety ratings, but maternity had the poorest.
A little drop has occurred since then.
Seven out of ten units may not provide adequate safety.

privilege
Hannah and midwife Phoebe Isaac have many interests and experiences.
Their descriptions of the moment a kid is born are remarkably similar, right down to the body language they use.
Their faces brighten, and they each say “privilege” with the same accent.
The 22-year-old Phoebe wants this to be her permanent career after qualifying last summer.
But Hannah quit her beloved work when she was 35 years old.
When taken as a whole, recruitment and retention capture the essence of the midwife crisis as well as its potential remedies.
Dream job
Phoebe, who proudly declares herself “the future of midwifery” according to her boss, is enjoying her dream job and is grateful for the assistance she has received since becoming a midwife.
With a large number of midwife positions vacant, the Croydon unit is making great efforts to fill them.
Forty full-time positions were available at this period last year.
By bringing in fresh faces like Phoebe, we hope to reduce that number to 20 by March.
However, in order to fill up rota gaps and ensure the safety of moms and babies, the team must utilise agency staff.
‘I miss it but I mourn it’
Hannah, who has experience working in a maternity centre in another region of the nation, wants to emphasise that midwives like her always give it their all.
However, she recounts instances where she was overburdened with the care of multiple mothers and infants due to staffing shortages.
“I walked away from it because I couldn’t live with myself if I provided unsafe care for someone because the staff numbers were unsafe,” she adds, her voice barely audible, despite her conviction that she always managed to keep them safe.
It was great. I love it. On the other hand, I lament it since I don’t see any signs of improvement.
Midwife shortages
Despite a decline in the overall birth rate, the complexity of individual deliveries is on the rise.
The percentage of caesarean sections performed has increased from 13% a decade ago to 23% today.
This necessitates additional time spent in the hospital and the assistance of midwives during the delivery process.
A long-standing problem, according to Royal College of Midwives (RCM) chief executive Gill Walton, “huge gaps in midwifery staffing levels” occur when maternity services are not given the priority they deserve.
She continues: “What we’re asking for is not to be at the back of the queue, not to be overlooked.”
Finding a happy medium between training new midwives and keeping the ones we have is no easy task.
The RCM is concerned about a self-perpetuating cycle wherein current midwives may feel burnt out and opt to leave their positions due to the increased workload caused by staffing shortages.
It is imperative that we retain our current midwives and recruit more of them. Among the most rewarding careers you may have is that of a midwife. And we must ensure their well-being,” Gill adds.
Posts unfilled
We submitted a Freedom of Information (FOI) request to 106 trusts that have maternity units.
We inquired about the number of full-time midwife positions they had budgeted for in the summer of 2023, as well as the number of vacancies in those positions.
Across trusts, there were 25 vacant midwife positions, making up 11% of the total jobs.
Several trusts experienced significant shortages, with the highest reaching 35%.
FOI requests from Wales and Northern Ireland revealed that staffing concerns are less prevalent compared to England. In these regions, the average percentage of vacant midwife positions stands at 6% and 9% respectively.
Scotland’s figures indicate a smaller gap of 4%, but it utilises a different method to record workforce data compared to the other nations.
‘Things are already improving’
Efforts to increase the number of midwives being trained and hired are already showing positive results.
The government aims to boost the number of midwives in training by 13% over the next few years.
The Department of Health and Social Care has made significant investments to enhance maternity and neonatal care, with an annual budget of £165m. This funding is set to increase to £186m in the near future.
England’s Chief Midwifery Officer Kate Brintworth remains hopeful about what lies ahead.
She claims that there have been noticeable improvements. We now have an additional 700 midwives in their positions. Our retention rates are on the rise, and staff are beginning to experience a more positive atmosphere.



More Stories
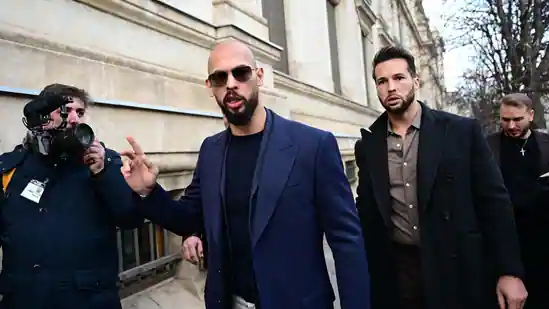
Trial for Rape and Human Trafficking will take Place in Romania for Andrew Tate and his Brother Tristan
A British individual tests the first Customised Melanoma Vaccination
Gaza Baby Delivered from Dead Mother’s Womb Perishes